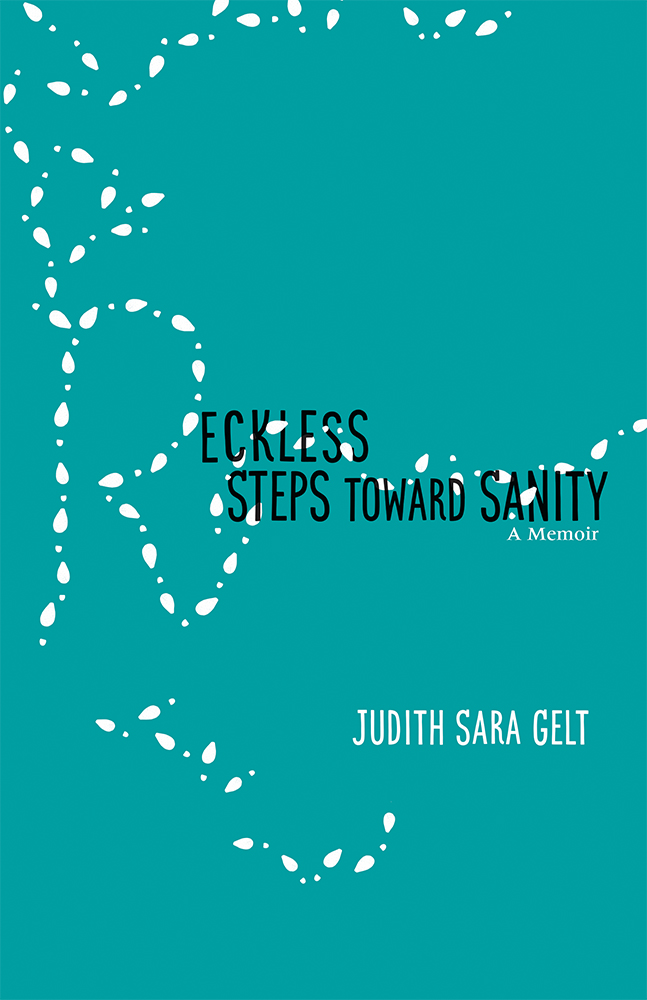
Judith Sara Gelt: Reckless Steps Toward Sanity

Judith Sara Gelt
The views and opinions expressed in following story are those of the author and do not necessarily reflect the opinions of Mental Health Colorado.
I grew up in a home invaded by bipolar disorder that stuck fast to my mother, a woman who suffered from the time she was 54 until she died at 97. My father, a man who needed to control his world, was confused, angry and mean. Her illness didn’t pay him any mind. And, residue from major depressive disorder has clung to me since my early 40s. In my memoir (Reckless Steps Toward Sanity, University of New Mexico Press, 2019), I describe my feelings about my depression—
This was serious depression, wasn’t it? I knew the stigma fastening itself to the diagnosis. Society added (sadly, can still add) “disgraceful” to major depressive disorder’s list of attributes. It wasn’t a disease. I would be treated by a psychiatrist, a shrink, and respectable doctors weren’t tagged with nicknames. And wasn’t “being depressed” the same thing as “feeling really sad”? Come on. Everyone gets sad. Pull yourself together! Go for a walk, you’ll feel better. Each appraisal took away another piece of already-defeated me.
It can feel as though you’ve been blamed for making a dreadful mistake. Clinical depression stains your skin, so you can’t slip it off, hide it in a drawer. Less that ugly sweater choice and more the hideous tattoo decision that you strategically cover with clothing. In some cases, you can conceal your suffering. If you can possibly walk, it’s upright; if you can talk at all, you make conversation and take care of business; if you can muster laughter, it sounds sincere. You fake sleepwalk: eyes wide, wide awake, but no one there. This way others don’t insist, “What’s wrong? What’s happened?” Since, of course, everything is wrong and nothing has happened. Except you long to be in your bed more than anything in the world. More than being with your child.
Still, my mother’s bipolar depressions were more agonizing than my singular depressions. Hers began when I was 14, and often chained her to bed for days and days, her wails choking the hallway, “I’m a terrible mother. I’m so sorry. A terrible mother.”
My experience for the past 27 years is with antidepressants, and then combinations of antidepressants, and then antidepressants in combination with other meds that act like antidepressants.
I’m a willing patient. In fact, I celebrate having recently found a psychiatrist who insists she will work to find the right medications to get me feeling better. To feel like myself again. Or close. She’s tenacious. And that counts with me.
When I was 16, I wasn’t suffering from major depression disorder, but inundated by hopelessness and absent control over my circumstances, I wanted to die. And, when my attempt didn’t work, and I was in the hospital, I tried again. There are cries for help, but I attempted suicide to end my life, to end the pain of living it. Two years earlier, circumstances had collided in dangerous ways, and the shrapnel slashed deep with no one there to stitch my wounds and make it better. My mother had disappeared into a hospital, and my father never managed to explain what was happening to her. He barely dealt with his own pain. We never spoke about, well, anything, and there were no relatives or family friends to check on us. My father must not have been in touch with anyone. And, no one saw through the pretty veneer of our upper-middle class home.
Eventually, I went to a trusted teacher for support and attention, and he assaulted me. That was the day I swallowed pills.
After my attempted suicide, I remained inside the hospital. At first, I wallowed in deep despair after finding myself alive, but I followed “orders.”
They welcomed me to the Ts. It was 1968.
- Occupational therapy. I thought patients would be acquiring skills to prepare them for occupations. Yet, I remember long wooden tables strewn with what I knew to be arts and crafts. As a little girl, I had treasured building popsicle-stick houses, pressing images into shiny tinfoil reliefs, braiding plastic lanyards and weaving oven mitts. Apparently, here the designation meant “keep patients occupied.” Fine by me.
- Recreational therapy also wore a disingenuous label. Recreational warfare was more precise. A net. A volleyball. The other patients—teenagers, a few even early twenties, a few decidedly psychotic. The ball was the missile. The players were either launchers or targets. I was a target and was convinced the staff performed as cheerleaders ignoring all casualties. If I lunged to return a ball aimed at my head, stinging, strawberry circles formed on my forearms. If I cowered, and I spun or ducked, purple blossoms bloomed on my back or shins.
- Group therapy consisted of chairs in a circle in a sizeable, otherwise-empty room. A doctor sat in one—the shrink, a strange stranger. The other chairs were for us, so we could “dis- cuss.” I recall no words, only the voices of other patients, whom I also didn’t know.
I don’t remember my voice. Ever.
Finally, there were the individual therapy sessions. Perhaps those were labeled IT. Compared to everything else, they were “it” for me. In his private office down one of the hallways, my doctor sat in a chair, and I perched on the edge of a couch across from him. We met often, perhaps every day. I craved a way to stop existing between unbearable life and no life at all.
The idea of a tolerable existence drifted, and I couldn’t hold on, couldn’t pull it close enough to trace its contours, detect safe terrain. And how to explain the pills, my past, my feelings? Where would I unearth the words? Regardless, I must have listened while he talked, and I must have talked while he listened.
Over time, possibility plowed through hopelessness.
It was my assigned psychiatrist who saved me. It took a while, but he delivered the notion that things could get better. He showed me I had some control. And eventually, I believed he cared, even loved me. Those three elements—hope, control, and trustworthy love—these saved my life. My doctor did this for me, and I remain a fan of psychiatry and “talk” therapy as well as medication for serious mental illness and suicidal tendencies if dynamic doctor and patient matches are made, and with patients and medications as well. No matter how long that takes. I’m convinced other methods are also viable. Somehow, as each of us who suffers mental illness is assigned to a treatment, there is some luck or fate or faith at work.
I’m grateful for the doctor I was assigned when I was an adolescent, plus all of the therapists and psychiatrists and medications that have helped me be well as an adult with a daughter of my own. If everyone suffering mental illness could be given the opportunities I was. If they could have my advantages—to be rescued before they died, to have enough money or insurance so they receive good care. This is my hope for the future. I can write about what happened because my hope was returned with the help of experts and their interventions.
Reckless Steps toward Sanity: A Memoir
Excerpts from Reckless Steps toward Sanity: A Memoir by Judith Sara Gelt. Copyright © 2019 University of New Mexico Press, 2019.
———————————————————–
DONATE TO MENTAL HEALTH COLORADO
More than 500,000 Coloradans lack the mental health care they need. You can change that. For more than 60 years, Mental Health Colorado has led the charge in promoting mental health, ending stigma, and ensuring equitable access to mental health and substance use services. It’s life-changing work. Your contribution makes it possible.